Mucus-loving gut bug could be key for controlling cholesterol, lab study finds
A study conducted in lab dishes and mice finds that mucus-eating bacteria found in the human gut could be key for controlling cholesterol.
Bacteria that feast on mucus in the human gut may prove useful in controlling cholesterol levels, a new study conducted in mice and lab dishes suggests.
Akkermansia muciniphila is a bacterium that lives in humans, and primarily in mouse studies, the microbe has been linked to protection from metabolic diseases, neurological disorders and certain infections. As its name suggests, A. muciniphila mostly consumes mucins — large, sugar-rich proteins that form the bulk of the mucus that covers the lining of the intestines.
Because mucins are typically hard for microbes to digest, scientists were interested in investigating what enables A. muciniphila to colonize the human gut and thrive on the proteins.
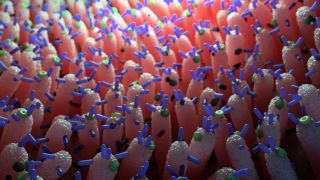
In their new study, published June 19 in the journal Nature Microbiology, the team first cultured A. muciniphila on mucin collected from pigs and observed the bacteria growing under a microscope. They saw that the bacteria were hoarding mucins in compartments within their cells, which the scientists named mucinosomes. Interestingly, these compartments seem to be specific to Akkermansia species, as they aren't observed in Bacteroides thetaiotaomicron, another mucin-loving microbe.
Related: People who live to 100 have unique gut bacteria signatures
The scientists then created mutant A. muciniphila strains using "transposon mutagenesis," a process that introduced genetic mutations in the microbes' DNA, and grew these mutants in mucin. Some mutants weren't able to produce amino acids, the building blocks of proteins, and these strains failed to multiply on the mucin, indicating that the production of amino acids is critical to the microbes' ability to benefit from mucins.
Next, the team fed mutant A. muciniphila to different genetically modified lab mice. The mutants' growth patterns in the cecum, a part of the large intestine, revealed that the bacteria that lacked the genes to produce amino acids had a really hard time proliferating, especially in the presence of other bacterial species. Genes for four specific amino acids — alanine, asparagine, glutamine and arginine — seemed especially important for A. muciniphila to successfully colonize the gastrointestinal tract.
In further mouse experiments, the researchers uncovered two groups of genes that are key for the transportation of mucin into the bacterial cells' special compartments. Dubbed mucin utilization locus (MUL) genes, they are critical for the bacteria's growth and their colonization of the gut.
The so-called MUL1 group of genes codes for proteins that transport mucin into the bacterial cells. The MUL2 gene group produces proteins that form pili — thin, hair-like appendages that protrude from the cell surface and likely also help transport mucin into the bacteria.
In "germ-free" mice bred to carry no gut bacteria, normal strains of A. muciniphila outgrew mutants with dysfunctional MUL1 or MUL2 genes when all the strains were made to commingle in the mouse gut. In addition, when grown in isolation, normal A. muciniphila suppressed the expression of mouse genes involved in cholesterol production, while the same cholesterol-making genes were jacked up in mice that carried A. muciniphila mutants with dysfunctional MUL1.
This showed that the mucin-gobbling bacteria could directly influence cholesterol production in the gut and could therefore serve as an important tool to curb high cholesterol levels, the authors concluded.
"This is an important and elegant study" that establishes a method for genetically tweaking A. muciniphila and shows how critical mucin is for the mucus-gobbling microbe's interactions with its host and with other bacteria, Willem Meindert de Vos, a professor emeritus at Wageningen University and Helsinki University who was not involved in the research, told Live Science in an email.
In a recent proof-of-concept study, de Vos and colleagues tried giving A. muciniphila as a supplement to human volunteers with insulin resistance and found that the volunteers' sensitivity to insulin improved and their cholesterol levels fell over time. However, that trial was very small, and more data on A. muciniphila supplementation in humans is still needed.
Live Science newsletter
Stay up to date on the latest science news by signing up for our Essentials newsletter.
Soumya Sagar holds a degree in medicine and used to do research in neurosurgery at the University of California, San Francisco. His work has appeared in New Scientist, Science, Discover, and Mental Floss. He is a passionate science writer and a voracious consumer of knowledge, especially trivia. He enjoys writing about medicine, animals, archaeology, climate change, and history. Animals have a special place in his heart. He also loves quizzing, visiting historical sites, reading Victorian literature and watching noir movies.
Most Popular
By Harry Baker
By Kiley Price